Providing professional care in fertility, gynaecology and minimally invasive surgery
Ectopic Pregnancy
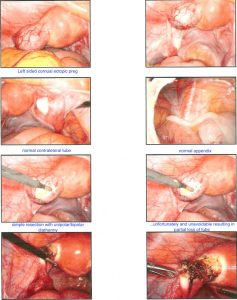
Ectopic pregnancy is defined as a “developing embryo implanting at a site other than the cavity of the uterus”. The embryo may attach to any surface within the abdomen or pelvic cavity. 98% of the time that surface is within the fallopian tube. This is sometimes called a tubal pregnancy. Rarely, the developing embryo may attach to another site such as the cervix, ovary or within the join between the fallopian tube and uterus. This is called an interstitial or cornual pregnancy. Rarely, a so-called heterotopic pregnancy may occur, where a twin pregnancy, implants one within the fallopian tube and one within the endometrial or uterine cavity. This is more common after a double embryo transfer, in women undergoing infertility treatment.
Why is ectopic pregnancy dangerous?
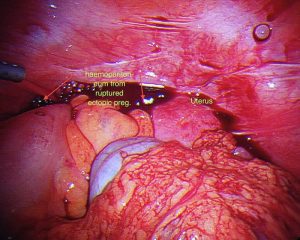
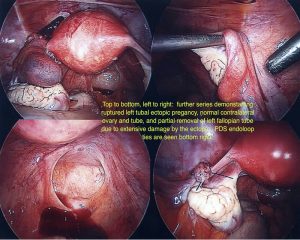
Embryos that do not implant in the uterine wall are unable to develop normally ad cannot end in a healthy term pregnancy. Usually the embryo has already stopped developing at the time of diagnosis. Unfortunately an ectopic pregnancy cannot Ectopic pregnancies may cause rupture of the organ in which they are implanted, typically the fallopian tubes. This generally leads to slow, prolonged bleeding although in some situations may cause rapid bleeding. Rapid blood loss such as this has resulted in maternal death. This still happens but is very unlikely as ectopic pregnancies are nowadays diagnosed much earlier and treated expeditiously.
What causes ectopic pregnancy?
The following factors have been identified as causes of ectopic pregnancy. Sometimes more than one, or none, may apply:
- Abnormalities of the fallopian tubes. If the fallopian tubes are damaged or abnormal as a result of previous infection (typically pelvic inflammatory disease) endometriosis, surgery, tumours or rarely due to malformations present since birth there is an increased risk of ectopic pregnancy. Surgery to reconstruct the fallopian tubes after tubal ligation can also increase the risk of ectopic pregnancy. The previous infection concerned, may not have been noticed by the patient.
- Previous ectopic pregnancies. The base line risk of ectopic pregnancy is around 1:100 however this increases to 1:10 if a previous ectopic pregnancy has been diagnosed.
- Previous genital or pelvic infections. Pelvic infections, Gonorrhea or Chlamydia are a major cause of tubal problems, scarring and adhesions, which increase the risk of ectopic pregnancy. Note that conditions such as appendicitis and endometriosis can do likewise.
- The incidence of ectopic pregnancy high in women with infertility most likely due to an increased incidence of tubal abnormalities. Fertility drugs may also increase the risk in this population.
- Multiple sexual partners. Having more than one sexual partner is associated with an increased risk of pelvic infection and therefore an increased risk of ectopic pregnancy.
- IVF treatment (in vitro fertilization). This is associated with both an increased risk of ectopic and heterotopic pregnancy.
- Tubal ligation. Tubal ligation is a surgical procedure in which the fallopian tubes have been cut, clamped or burnt in order to prevent further pregnancies. Since the tube is made of living tissue, sometimes a tiny hole occurs adjacent to the point of occlusion, which means that a pregnancy is possible. A pregnancy in this case, is commonly within the fallopian tube hence an ectopic pregnancy. The risk of an ectopic pregnancy after tubal ligation does not decrease with a period of time.
- Intrauterine contraception devices.. Women who become pregnant whilst using an IUD have a slightly higher risk of ectopic pregnancy. This means not that ectopic pregnancies are more common however a greater proportion of pregnancies are ectopic in this situation.
- Smoking
Ectopic pregnancy symptoms: How might I know that I have an ectopic?
The most common symptoms of ectopic pregnancy include, abdominal pain, a missed or altered last period, vaginal bleeding which may be minimal in combination with symptoms of early pregnancy such as breast tenderness, frequent urination or nausea.
In days gone by ectopic pregnancies more frequently presented after collapse of the patient due to blood loss, but thankfully this is now rare. The most common symptoms are slight abdominal pain, an abnormal period, and a slowly rising beta hCG, (pregnancy hormone.) Around 50% of women have no symptoms until the fallopian tubes bleeds.
What are the consequences of ectopic pregnancy?
Ectopic pregnancies can sometimes resolve on their own, however, the consequence of an ectopic not resolving and progressing to rupture or intra abdominal bleeding is so severe that waiting for an ectopic pregnancy to resolve is not recommended treatment. As soon as an ectopic pregnancy is diagnosed it should be treated.
Ectopic pregnancy diagnosis
Ectopic pregnancy can be difficult to diagnose. Sometimes, they form when the pregnancy is so early that they cannot be seen on an ultrasound. However a combination of Beta hCG, blood tests, ultrasound and examination are helpful. Sometimes a laparoscopy is required to diagnose an ectopic pregnancy.
Ectopic pregnancy treatment
An ectopic pregnancy must be treated in order to stop its growth and prevent complications. Treatment is broadly divided into medical treatment and surgical treatment.
1. Medical treatment
Methotrexate is a very successful treatment for ectopic pregnancy. It you use Methotrexate an ectopic pregnancy must fulfil several criteria, which I will explain to you. Therefore Methotrexate is not appropriate in all the patients. However it can be a useful way of causing an ectopic pregnancy to resolve without surgery.
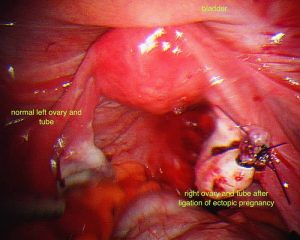
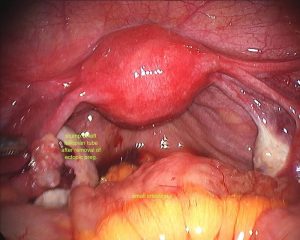
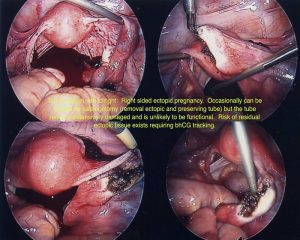
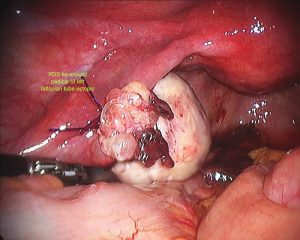
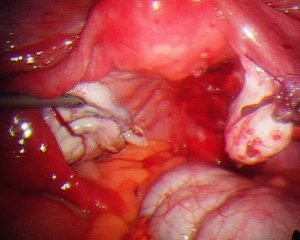
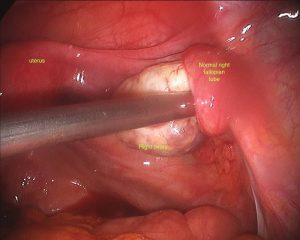
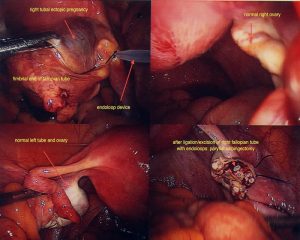
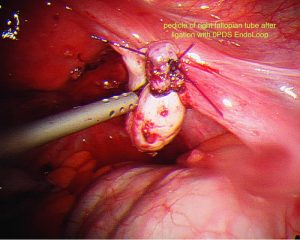
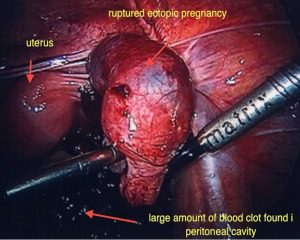
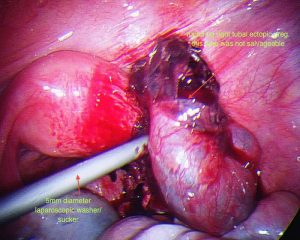
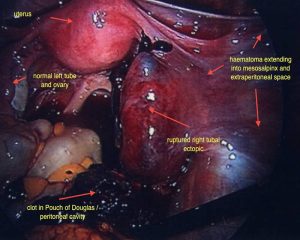
2. Surgical management
Surgery is still the mainstay for treatment of ectopic pregnancies. This should invariably be done via a laparoscope. A skilled surgeon can deal with even a ruptured ectopic pregnancy, where there is a lot of intra abdominal blood, laparoscopically. It should rarely or never be needed to perform a laparotomy on someone with an ectopic pregnancy. Sometimes, Methotrexate treatment may fail, resulting in subsequent surgical treatment. It is important to realize, that this is not so much a failure of treatment or reflecting a poor treatment choice however this reflects appropriate judgment when the desired response to Methotrexate is not gained.
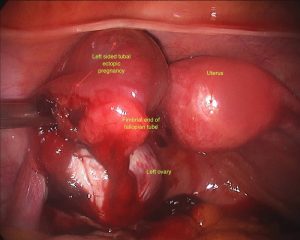
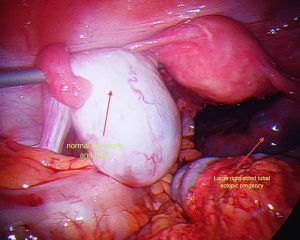
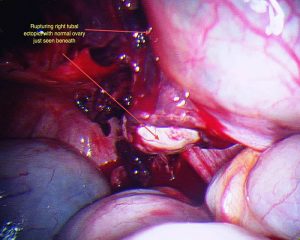
Will my fallopian tube be removed?
During surgery it is sometimes possible to remove an ectopic pregnancy from the tube (called salpingostomy) It is nice to perform this if the woman would like to become pregnant in the future, however this is not always possible as the tube is usually extensively damaged by the ectopic pregnancy. In most cases, mainstream management is removal of the fallopian tube. It is important to remember, that a fallopian tube affected by an ectopic pregnancy, is rarely of use in the future and will probably cause further ectopic pregnancies on that side.
Consequences of removing a fallopian tube
Surprisingly, removal of a single fallopian tube does not greatly decrease fertility. I am often asked if it means a woman can only fall pregnant every second month, however the fallopian tube on the opposite side is easily able to reach across the pelvis to pick up eggs from the other ovary. When the ectopic pregnancy is diagnosed and removed surgically, the ovary of the same side is left intact. It is surprising, that in around 10-20% of cases, one sees an ovarian cyst, from which the lady ovulated in order to form the pregnancy on the opposite side to the ectopic pregnancy proving this point.
Hospital stay
Duration of the hospital stay often reflects the pre operative state in which the woman arrives in theatre. If she has been sick or presented to hospital acutely unwell, then although the laparoscopic surgery for treatment for ectopic pregnancy is very simple, an overnight stay might be required.
Sometimes a blood transfusion is required after the operation or during an anaesthetic however this is unlikely.