Providing professional care in fertility, gynaecology and minimally invasive surgery
Endometriosis
What is endometriosis?
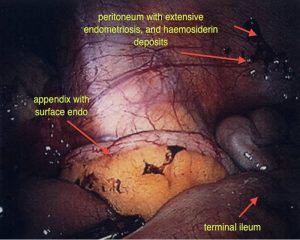
Endometriosis refers to the presence of abnormal glands that normally line the uterus, outside the uterine cavity. Typically this occurs in the pelvis but it may occur in virtually any part of the body. The most common locations for endometriosis are the outer surface of the ovaries, the pelvic peritoneum (the tissue that lines the abdomen), the uterus, fallopian tubes, bowel or bladder.
How common is it?
Endometriosis is found in around 40% of women who are having difficulty conceiving and around 15% of the population.
Is all endometriosis the same?
Endometriosis most likely represents a diverse spectrum of disease, which affects different women in different ways. Some women may have quite severe endometriosis and are virtually without symptoms whilst others have milder endometriosis and have obvious symptoms or difficulty conceiving. There is a complex interaction between the endometriosis tissue and the woman’s body, which is not completely understood.
Why would I get endometriosis?
The following factors may increase your chance at developing endometriosis.
- No pregnancies resulting in the birth of a child.
- Endometriosis in a woman’s mother or sister.
- Short menstrual cycles (less than 27 days) with prolonged flow (more than 8 days).
- Partial or complete obstruction of normal menstrual flow, e.g., from uterine abnormalities such as a tight cervix, vaginal septum or uterine fibroids.
- White or Asian race.
Conditions that decrease the amount or frequency of menstrual bleeding may lower the risk of endometriosis, e.g., pregnancy or prolonged use of the oral contraceptive pill.
Causes of endometriosis
The cause of endometriosis is not known. However, several theories have been suggested:
- Retrograde menstruation is a theory proposed by Sampson in the 1920’s. It states that menstrual blood flow and tissue flows backwards through the fallopian tubes into the pelvis. Retrograde menstruation is often observed during a laparoscopy, when the woman has her period, however not all women develop endometriosis. This means that there is a complex and incompletely understood relationship between the endometriosis tissue and the woman’s pelvis, which enables the disease to progress. However, endometriosis has been observed after tubal ligation (clipping of the tubes) and so clearly retrograde menstruation cannot be the entire answer. It is likely that subtle changes in the immune system, or the endometriosis tissue’s ability to produce new blood vessel growth, may be the factors involved in progression of endometriosis.
- Endometrial tissue from the uterus might be transported through the blood or lymphatic vessels to distant sites within the pelvis. This explains how endometriosis can sometimes be found in sites that do not have any close physical proximity to the uterus or fallopian tubes.
- Coelomic metaplasia is a concept that states that the cells lining the abdomen and surface of the ovaries may change, of their own accord, into endometriosis tissue under the influence of certain factors, which may include retrograde menstruation or infections.
Symptoms of endometriosis
Those with endometriosis may have no signs or symptoms. In those who do have symptoms, the intensity and location of the pain does not always correlate well with the severity or location of the endometriosis. It is possible to have referred pain from endometriosis, e.g., pain at a distant site.
For many women, severe pelvic pain or pain during periods is their main symptom. The pain typically occurs around the time of the period, during or after sex, with a full bladder, on passing water or on using the bowels. Spotting between periods, frequent or heavy menstrual flow and pain that does not respond to the use of the contraceptive pill and simple analgesics are all strong indicators of endometriosis. Pelvic pain is probably the result of bleeding from areas of endometriosis within the pelvis and “inflammatory mediators” such as prostaglandins and interleukins, which may also be implicated in difficulty conceiving.
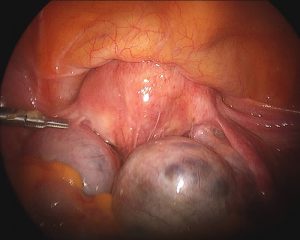
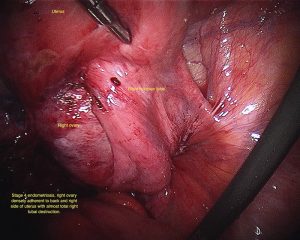
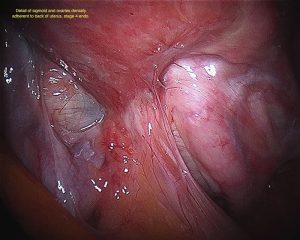
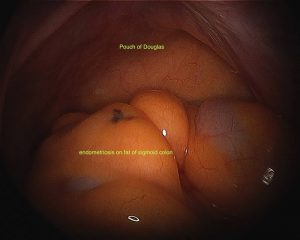
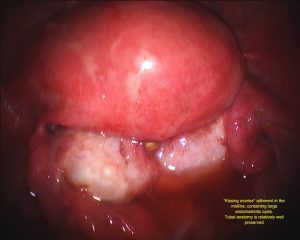
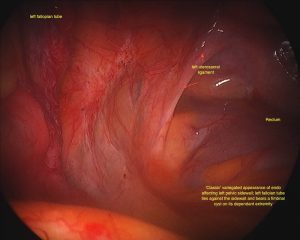
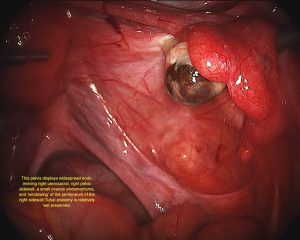
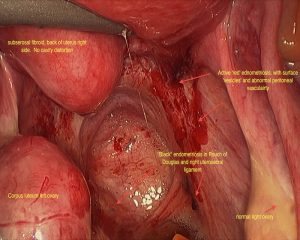
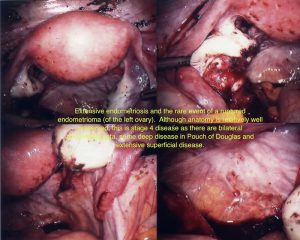
Endometriomas and Deep Infiltrative Endometriosis
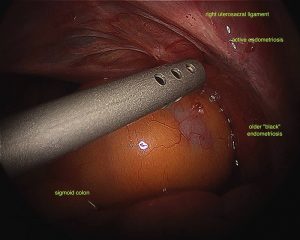
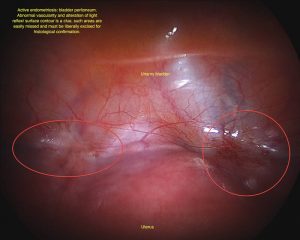
Endometriomas are areas of endometriosis that are large enough to form a cyst on the ovaries. The endometriosis cyst contains a brown liquid that has the appearance of melted chocolate, hence the alternative name “chocolate cysts”. Chocolate cysts have a characteristic appearance on ultrasound scan however unless cysts or very major endometriosis is present, ultrasounds are not good at diagnosing endometriosis as a general rule. Deep infiltrative endometriosis (DIE) is a name given to endometriosis that has spread through the lining of the pelvis or other tissues and is infiltrating the structures beneath such as the ligaments supporting the uterus, the bowel, bladder or other structures.
Diagnosis of Endometriosis
There are unfortunately no blood tests or imaging studies that can make a definite diagnosis of endometriosis however this is done by laparoscopy and submission of a sample of endometriosis to the pathology service. Endometriosis is rarely diagnosed before a girl’s periods commence or after the menopause. Laparoscopy for exploratory surgery is the definitive way of diagnosing endometriosis. Without this, the diagnosis is only assumed.
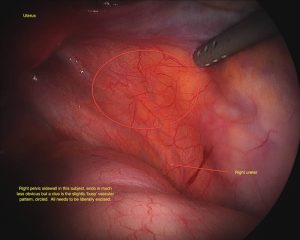
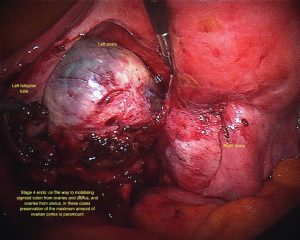
Staging of Endometriosis
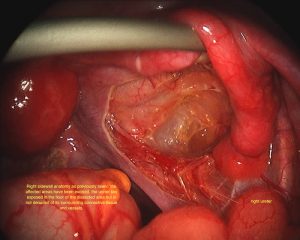
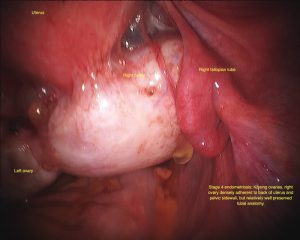
Various staging systems for endometriosis have been proposed. The most commonly used is the American Society For Reproductive Medicine (ASRM) staging system, which is a good descriptive method however does not correlate closely with the effect of the endometriosis on a woman’s fertility. Stages are 1 to 4. There are also anomalies within the scoring system (see image library) that means that you may have stage 4 disease that doesn’t look very extensive.
Treatment of endometriosis
There are several treatment options for women with endometriosis and the kind of treatment embarked upon depends purely on a woman’s wishes, her desire for fertility, the desired effects and the wish or not to be on long-term medication.
Analgesics
I would consider it unsatisfactory to use these as my first line treatment after a positive diagnosis of endometriosis. Most women come to me having already tried the oral contraceptive pill in combination with analgesics to free themselves from pelvic pain. Once a diagnosis is made then an attempt should be made to cure the endometriosis.
Oral Contraceptive Pill
The oral contraceptive pill contains both oestrogen and progesterone. When taking the pill for a while the effect on the lining of the uterus is generally to cause it to think substantially which results in much lighter periods. However, it never really disappears. The same effect occurs with endometriosis in that the endometriosis is suppressed without ever really disappearing. Nonetheless, if disease is mild, the oral contraceptive pill can be a useful and physiological way of suppressing pain symptoms without causing any real harm. The therapy can be continued for a long time, generally without side effects.
Other Forms of Hormonal Therapy
Other forms of hormonal therapy similarly seek to suppress endometriosis. This would include progesterone tablets, progesterone injections, Danazol or gonadotropin releasing hormone analogues. None of these are without significant side effects and none are generally taken for a long period of time for reasons of cost, convenience and side effects.
Surgery
In my hands, surgery is the mainstay of treatment for diagnosis and treatment of endometriosis. Many treatment modalities have been described in the past and all have their advantages and disadvantages. The exact type of surgery that is required depends on the extent of a woman’s symptoms, her desire for fertility, the site and radiation of the pain and the potential risks and benefits of surgery.
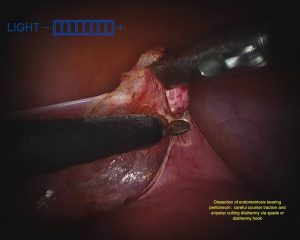
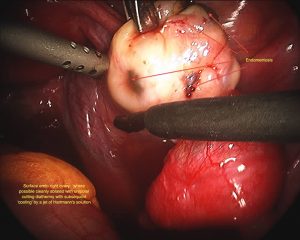
Excisional Surgery
Excisional surgery refers to cutting out the deposits of endometriosis. This requires greater time and skill and is ideally suited to those in whom the endometriosis is severe, resulting in adhesions, sticking together of tissues and distortion of anatomy. If the endometriosis is deep then excisional surgery is really the only kind that can be carried out with the hope of obtaining adequate cure.
Ablative Treatment
Ablation refers to burning or destroying endometriosis deposits. This can either be done with electrical energy or laser. Laser treatment had a vogue in the 1980’ and 1990’s however the technology is expensive, difficult to use and cumbersome. Ablative therapy typically works best where lesions are small and superficial however in the presence of deep disease, disease clearance is much less likely.
Other Issues In Surgical Treatment
The vast majority of endometriosis should be treated by laparoscopic approach. In rare cases laparotomy (opening of the abdomen through a large incision) may be necessary when dealing with extremely extensive adhesions or invasive endometriosis involving the ureters, bladder or rectum. Indicating for removing endometriosis on such structures really depends on a patient’s symptoms and plans for fertility. Removal of deep, infiltrative endometriosis involving the bowel is an extensive procedure requiring removal of a short section of bowel and often has associated bowel disturbance thereafter for many months. Pain relief is achieved in most patients who undergo laparoscopic resection of endometriosis however the risk of recurrence is estimated to be up to 40% at ten years follow up and around 20% of patients may undergo additional surgery within two years. Success rates in relieving pain are most marked in those who have severe, e.g., stage IV disease and such women often feel a reduction in pain in the immediate post-operative period.
Definitive Surgery
Definitive surgery involves a hysterectomy with or without removal of the fallopian tubes and ovaries. Removal of the ovaries in a pre-menopausal lady is a matter not to be taken lightly however if they are heavily involved with endometriosis and are likely to form adhesions resulting in ongoing pain or the requirement for further surgery, then removal of the ovaries is sometimes required. The decision to proceed to a hysterectomy is primarily dependent on the patient’s interest in having (more) children.
Hormone replacement after hysterectomy for severe endometriosis
If the ovaries are removed in a premenopausal lady then oestrogen replacement with or without progesterone to prevent menopausal symptoms and loss of bone density, should be considered even if surgery has not removed all the endometriosis. There is a very low likelihood of symptom recurrence in these cases (less than 5%) except if endometriosis involves the rectum. It is not known whether the use of progesterone will reduce the chances of any residual endometriosis growing again. This theoretical benefit of avoiding a small risk of recurrent disease must be balanced against a small increase in the incidence of breast cancer.
Reasons for combination medical and surgical therapy
Pre-Operative Medical Therapy
Hormonal suppression such as with GnRH analogues (Zoladex and others), has been used prior to surgery to try to decrease the amount of adhesions and make the endometriosis less biologically active (“sticky”) thereby facilitating the surgery. However, there is no evidence that this results in a better operation and in the vast majority of cases a competently performed primary operation with attention to detail in clearance of disease, is far preferable.
Post-Operative Medical Therapy
Previously, progesterone or tablets such as Danazol or GnRH analogues have been used in conjunction with surgical clearance of disease in order to try to reduce disease recurrence. If, after surgery a woman still has pain with periods then certainly suppressing the menstrual cycle may be of benefit in reducing pain. However there is no increased chance of pregnancy (obviously impossible whilst the periods are stopped by tablets) and upon ceasing medical suppressive therapy, endometriosis will recur. My own approach is that if the woman requires contraception or if symptomatic relief has been incomplete after surgery, the most physiological approach is to commence and remain on the oral contraceptive pill. This is as good as more aggressive and expensive medications. There is evidence that insertion of a Mirena IUCD gives an additional benefit to a well-performed operation in terms of pain relief.
Endometriosis and infertility
This is a very complex subject and there is still much research being done on the matter. There is a complex relationship between endometriosis and infertility, which is due to the differing biological behaviour of the disease and different characteristics of patients. The mechanism for impaired fertility may involve anatomical distortion of the fallopian tubes or other pelvic structures and the production of chemicals substances, which create a hostile environment to ovarian function, ovulation, fertilization and implantation. There is no question that symptomatic endometriosis is best surgically treated prior to embarking on infertility procedures. Some women will fall pregnant when the endometriosis is removed however others may not. Nonetheless, it is important to rule out simple potential causes of infertility before embarking on an expensive and complicated treatment regimen such as IVF even though success rates are often high. The exact nature and extent of endometriosis clearance surgery must be tailored to a woman’s individual requirements. In older subjects who already have impaired fertility and may have extensive endometriosis on the ovaries, is currently thought (2009) that the most expeditious way of achieving a pregnancy is to proceed straight to IVF, although during the stimulation cycle extensive endometriosis may cause significant pain and discomfort.
In general then I recommend a thorough laparoscopic excision of all accessible endometriosis as part of the plan for addressing the causes of infertility. This will improve chances of falling spontaneously pregnant and will also improve your chance of success with IVF.
Treatment of Symptoms Related to Deep Infiltrative Endometriosis
Deep infiltrating endometriosis is a term used to describe endometriosis that has invaded deep structures such as the rectovaginal septum (space between the vagina and bowel), bowel, ureters, bladder or other pelvic structures. If disease is asymptomatic and merely noticed by doctor’s examination findings and fertility is not an issue, then the disease may be managed expectantly. Medical therapy of symptomatic patients is generally ineffective and only transient whereas surgical therapy is effective for relieving pain, dyspareunia and pain with use of bowels in many cases, however some studies suggest up to 40% recurrence of pain after eight years. Surgical resection of deep infiltrating endometriosis does not necessarily enhance future pregnancy rates. As mentioned above, if pregnancy is a primary goal, then proceeding straight to IVF is the most expeditious way of achieving a pregnancy. If the disease is symptomatic then the most effective current regimen may be surgical resection followed by three months of GNRH analogues, followed by IVF.
Conclusion
Endometriosis can be an enigmatic and difficult to treat condition. The mainstays of assessment are careful history, detailed examination and ultrasound scan and a well performed operation plus or minus post-operative medical therapy by the most simple and physiological means possible. Treatment of endometriosis in the presence of infertility must be tailored to a patient’s individual needs. Complete removal of known endometriosis definitely enhances spontaneous pregnancy rates however chasing more severe endometriosis that may involve operations with their potential for prolonged recovery phases, may not necessarily be required before embarking on fertility treatment. Pregnancy itself may improve the symptoms of endometriosis but does not cure it. Pregnancy provides a similar hormonal picture as remaining on the oral contraceptive pill and hence endometriosis is suppressed but not removed. During pregnancy a women has no periods and so pain from endometriosis may stop or be improved.
Questions to ask your doctor about endometriosis
I encourage you to be very selective about whom you choose to operate on your endometriosis. If you have endometriosis, have a family history endometriosis or think that you may have endometriosis due to your symptoms it makes sense to see a doctor who treats endometriosis on a frequent basis.
You should consider the following:
- What treatment method does your doctor advise for endometriosis?
- How do you measure the outcome of your treatment or surgery and for how long does your doctor follow their patients?
- If the initial treatment is unsuccessful what does your doctor recommend as a subsequent course of treatment?
- Does this treatment approach temporarily help your symptoms or actually remove the disease?
- What proportion of patients get a second operation within a year?
- Does your doctor recommend diathermy burning, excision or lasering of endometriosis and why?
- Will the procedure be performed via laparoscope or laparotomy?
- Will photos and videos be taken of your operation and be presented to you with an explanation after the procedure?
- Will biopsies of all endometriosis specimens be taken and sent to pathology for verification?
- If a hysterectomy is eventually needed will this be performed via laparoscopic or open approach?
- What is your doctor’s specific training and ongoing interest in the endometriosis surgery?
- If the endometriosis lies over the ureters or involves the bowel, will this be corrected?